retinal detachment
Retinal detachment is a serious condition, in that even after surgery, its prognosis is necessarily limited, whereas without surgery, blindness is inevitable in the affected eye.
The disease is relatively rare : about 10000 cases in France annually (on average an opthalmologist examines three cases per year).
The name is self-explanatory : the eye's photographic film, or if you wish, tissue of pixels, detaches from the concave inner wall of this virtually spherical organ.
Medical science cannot say why, but is able to say how the retina detaches itself : retinal detachment is always preceded by a tear, or retinal hole, due to the detachment of the vitreous body, which with age, separates from the retina. Vitreous detachment is a physiological (normal) phenomenon which often occurs around the age of presbyopia (50) but sometimes much earlier (especially with myopes), or sometimes later. The vitreous detachment occurs in several phases ; it is normally asymptomatic, that is to say we do not notice it. It can cause floating specks, phosphenes (visions of fireflies or lightning), sometimes a rain of soot indicating intravitreal haemorrhage. So if you notice any of these symptoms, see a consultant as a matter of urgency, to detect any complication due to vitreous detachment, that is to say a tear or a hole in the retina, which will require laser treatment.
Statistically there are those who are predisposed to retinal detachment :
- starting with the short-sighted, especially those with significant myopia ; myopes have large eyes, and it is as if their retina (with a surface proportional to the square of the length of the eye) is weakening and cracking, showing specific aspects of retinal "lattice"
- secondly, there are those who have had cataract surgery
- and finally, those with eye injuries : perforation or even bruises.
Awareness of those with predisposition can help target the detection of dangerous retinal lesions (tears, holes, palissades), to treat them effectively, principally by laser, sometimes with additional cryotherapy (under local anaesthesia). This treatment therefore constitutes the preventive treatment for retinal detachment ; to be effective, it must be done according to a rigorous technique.
It is therefore logical to examine the retina of eyes of myopes when they have finished growing, that is to say around the age of 30, those potentially needing cataract operations, and those with traumatised eyes.
Since medicine is not an exact science, it often happens that people without any risk factor suffer retinal detachment ...
To this notion of predisposition, must be added triggering factors : prolonged and violent lightning, as experienced during the longest days (summer solstice), and the reflection of the sun on snow.
The symptom of retinal detachment is unequivocal : an opaque lunula on the corner of sight cuts progressively the peripheral vision of the eye, and within a few days, grows to give a dark cloud, which threatens the visual axis, and then covers it if consultation is delayed ; when all the retina is detached the eye cannot see anything, not even light.
Retinal detachment (along with cataracts) is not treatable by laser, but requires a surgical operation ; simple in its principle, often complex in it's realisation, and with uncertain results. It is treated as a semi-emergency, often after a day of rest in a position adapted to each detachment.
The goal is simple : to block up all the holes and tears.
The method uses two types of technique :
- the external technique, always preferable where possible, consists in sewing onto the wall of the eye a sort of bandage which acts as a support ; personally I use silicone sponge because it is a proven material
- the internal technique, more aggressive and risky, which involves removing a part of the vitreous body, to enable a bubble of gas to be injected into the eye, which holds things in place ab interno ; sulfur hexafluoride (SF6) which I use, remains in the eye for about a week.
The bonding of the retina at the back of the eye takes place by cryotherapy, sometimes supplemented by post-operational laser treatment ; if the volume of the sub-retinal fluid is too great to allow the occlusion of all the dehiscenses, it is punctured.
The operation takes between 45 minutes and two hours, and is achieved under either local or general anaesthesia.
The success rate in my hands is 90% -which means 10% failure- ; this performance which I check every year, conforms to the statistics of good specialist centres). The failures require a further operation. In practice, it is normal to be healed after one operation, but two interventions are not uncommon ; and even after three, if the retina is reattached, we shall all be very happy ; if not, in principle I consider the disease to have been stronger than the doctor, and we abandon matters.
The hospitalisation lasts a week ; the post-operative pain is moderate, and well controlled by systemic powerful analgesics ; but this disease is stressful, probably because of the uncertainty of it's outcome.
***
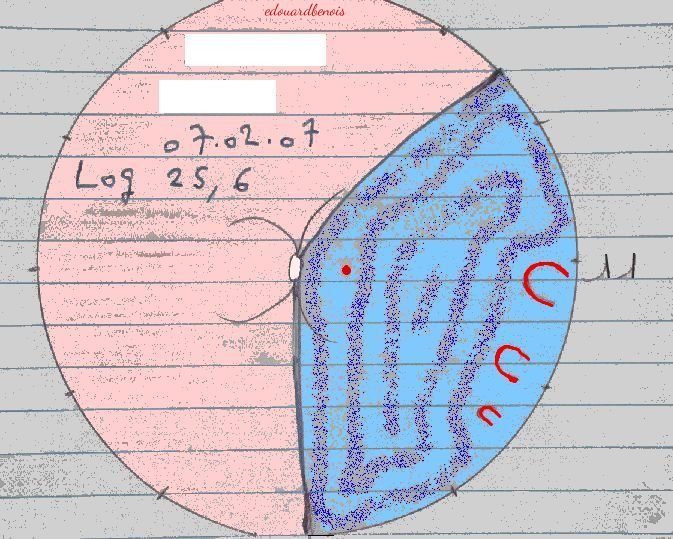
A problem well stated being half solved, the preoperative examination of retinal detachment is critically important ; the majority of surgeons would draw the detachments more or less as follows :
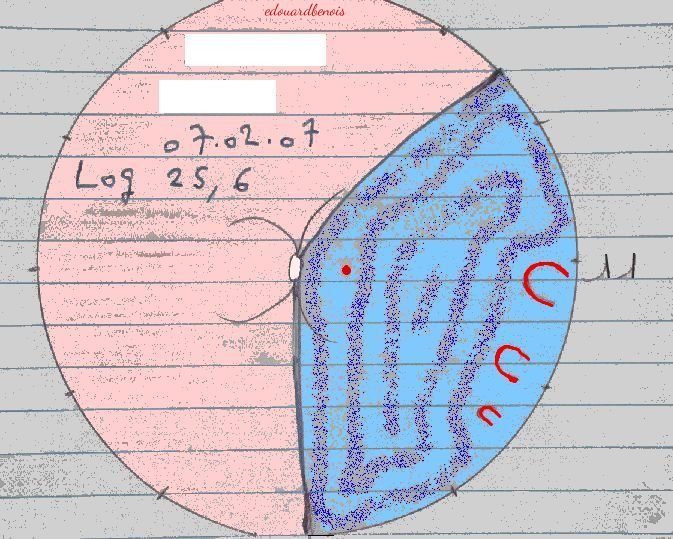
It can be said that this detachment lies between half past one and six o'clock. It is a left eye (front view), the number 11 (on your right) is on the side of the temple of the patient (his nose is on your left) ; this figure was written by the nurse during surgery, while this drawing was taped to the microscope, within my sight. The detached area is coloured pale blue, enhanced by my airbrush ; it includes the macula (the visual axis, that provides precise vision, marked by a dot surrounded by a small red circle), and is limited by the optic nerve (in the middle of the drawing) from which flow, very schematically drawn, the blood vessels of the retina. This separation, which involves a third of the area at the back of the eye, is due to three 'horseshoe' tears, aligned between three and half past four ; I noticed during the operation that their polar co-ordinates (the depth) was 11 mm from the boundary between the cornea (the transparent window through which we see the iris and the pupil) and the white wall of the eye. The pale pink area, the largest, is the part of the retina which remains attached and resembles the 'red eye' effect of photos taken with flash, which is easily erased by digital photo software. In the white rectangles were the first and last names of the patient, under those the date and the length of the eye (LOG = length of left eye), this being above normal, because the patient was myopic. This measurement helps to estimate the amount of fluid under the retina, and with other technical decisions.
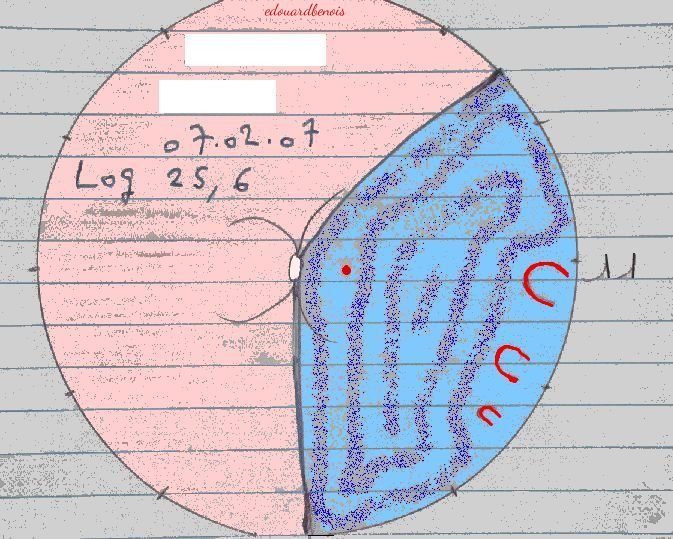
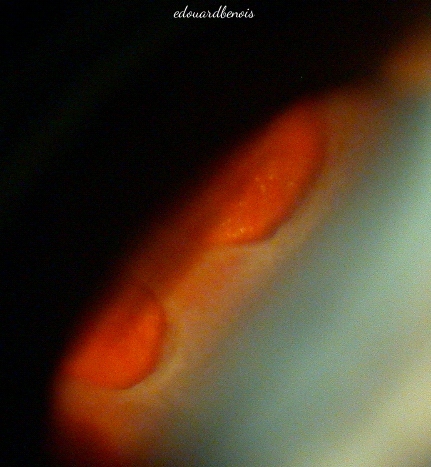
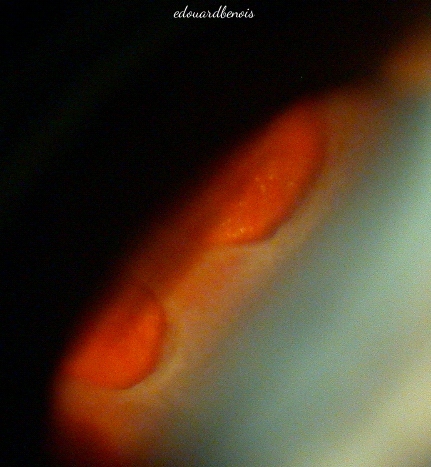
Here are the two largest tears (at three and four o'clock), photographed in a mirror leaning against a special contact lens (called 'three mirrors glass'), whose plane is tilted along the diagonal of the image leading towards the right : I could have flipped this with a photo software, but I preferred not to, to make you understand that we are obliged to imagine the reality, and to draw in mirror image.
***
"Health is a gift that we only appreciate when we have lost it, then regained it"
(proverb)
picture of a retinal detachment
home page
Thanks to Neville Trickett for translating this page :
if you find errors, it is my fault, since I made some modifications.